Superior Cluneal Nerve Entrapment
I. What is the Superior Cluneal Nerve?
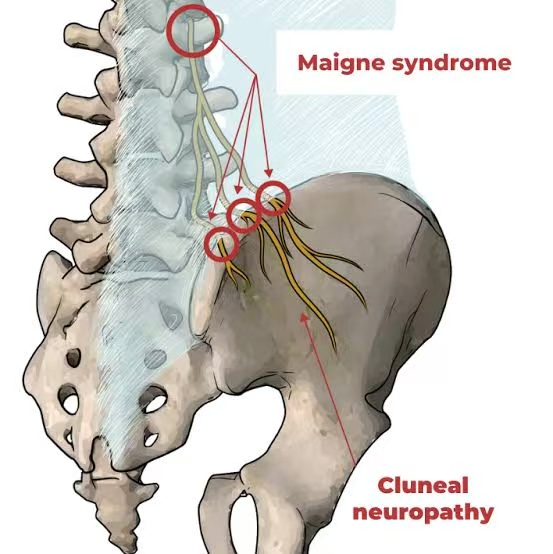
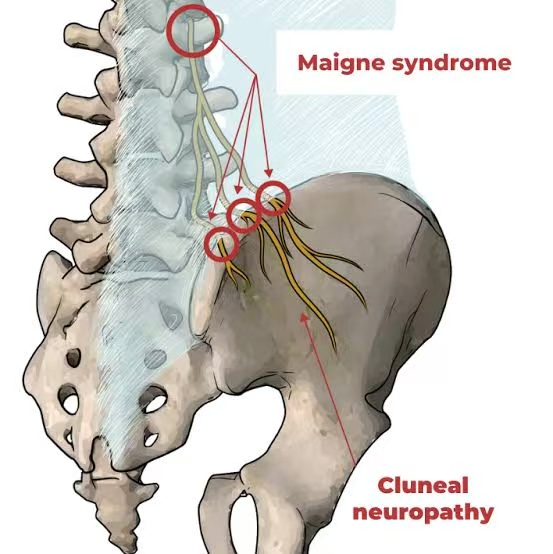
The superior cluneal nerves (SCNs) are cutaneous sensory nerves originating from the posterior rami of the first to third lumbar spinal nerves (L1-L3). These nerves traverse the thoracolumbar fascia, cross over the posterior iliac crest, and innervate the skin over the upper buttocks—hence the name “superior cluneal.”
Their main function is to transmit sensory signals from the upper gluteal region. They are not involved in motor control, but when compressed or irritated, they can cause significant pain and discomfort.
II. What is Superior Cluneal Nerve Entrapment?
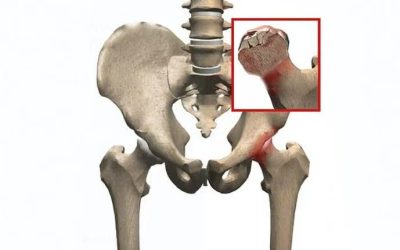
Superior Cluneal Nerve Entrapment Syndrome (SCNES) refers to a condition where these nerves become compressed as they pass through the thoracolumbar fascia or over the iliac crest, leading to chronic buttock pain that may radiate to the lower back or lateral thigh.
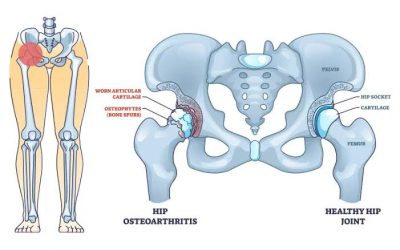
This syndrome is often misdiagnosed as sciatica, lumbar disc herniation, or hip joint disorders, but it is actually a peripheral nerve entrapment neuropathy, unrelated to disc pathology.
III. Pathophysiology
As the superior cluneal nerves pass through the fibrous tunnel formed by the thoracolumbar fascia and cross the iliac crest, they can become entrapped. Factors that contribute to this compression include:
- Anatomic variation
- Trauma (e.g., falls or impact)
- Post-surgical scar tissue
- Chronic myofascial tightness
- Abnormal posture
- Pelvic tilt or leg length discrepancy
These lead to nerve irritation, inflammation, and chronic pain.
IV. Typical Symptoms
SCN entrapment presents primarily with localized pain, characterized by:
1. Precise Pain Location
- The pain is located at the posterior iliac crest, typically 7–8 cm lateral to the posterior superior iliac spine (PSIS).
- Often unilateral, but may affect both sides.
2. Pain Characteristics
- Dull, burning, or stabbing pain
- May radiate to the lower back or lateral thigh, but not below the knee
3. Pain Triggers
- Worsens with prolonged standing, sitting, walking, or bending
- Palpation of the trigger point over the iliac crest often reproduces symptoms
4. Distinction from Sciatica
- Pain is higher up, over the buttocks rather than down the leg
- No numbness or weakness in the foot or calf
- MRI or CT scans are typically normal
V. Clinical Examination and Diagnosis
1. Physical Examination
- Palpation: Localized tenderness over the posterior iliac crest
- Positive Tinel’s sign: Tapping the nerve reproduction site triggers radiating pain
- Negative straight leg raise (SLR) test: Helps differentiate from sciatic nerve involvement
2. Imaging
- X-ray, CT, MRI: Used to rule out lumbar disc herniation, spinal stenosis, or fractures
- Often non-specific or normal findings
3. Diagnostic Nerve Block
- Injection of local anesthetic (e.g., lidocaine) at the suspected entrapment site
- Significant relief confirms the diagnosis of SCNES
VI. Treatment Options
1. Conservative Management
(1) Physical Therapy
- Heat therapy, ultrasound, electrical stimulation
- Myofascial release to reduce fascial tension near the iliac crest
- Use of massage guns, foam rollers, acupuncture, or manual therapy under professional guidance
(2) Exercise and Rehabilitation
- Stretching of gluteal muscles, quadratus lumborum, and iliopsoas
- Core strengthening to improve pelvic stability
- Leg length discrepancy correction with insoles if needed
(3) Medications
- NSAIDs (e.g., ibuprofen, celecoxib) for inflammation and pain
- B-complex vitamins to support nerve health
2. Nerve Block Injections
- Injection of local anesthetic + corticosteroid at the entrapment site
- Provides quick and effective pain relief
- Recommended early in the treatment course
3. Minimally Invasive Interventions
- Ultrasound- or fluoroscopy-guided nerve injections
- Radiofrequency ablation (RFA) for patients unresponsive to conservative treatment
4. Surgical Decompression (rare)
- Neurolysis or surgical decompression of the nerve
- Reserved for severe, chronic, and disabling pain not responding to other measures
VII. Prognosis and Self-Care Tips
SCN entrapment is highly treatable, especially with early diagnosis and intervention. Most patients improve significantly with conservative or minimally invasive treatments.
Self-care Recommendations:
- Maintain proper posture; avoid prolonged sitting or standing
- Regular stretching of hip and lumbar muscles
- Correct pelvic asymmetry or leg length differences
- Avoid trauma and overuse of the lower back and pelvis
VIII. Summary
Superior Cluneal Nerve Entrapment is an often overlooked cause of chronic low back and buttock pain. It is frequently misdiagnosed as lumbar disc disease or sciatica, leading to delayed or inappropriate treatment.
Recognizing the distinct location of pain, absence of neurological deficits, and response to local anesthetic injection are key to diagnosis. Conservative therapy is typically effective, and invasive procedures are rarely required.
If you suffer from upper buttock pain that does not respond to standard back treatments and imaging is unremarkable, SCN entrapment should be considered as a potential cause. Early recognition can significantly improve quality of life.